Health literacy skills
Introduction to Health Literacy
Definition of health literacy
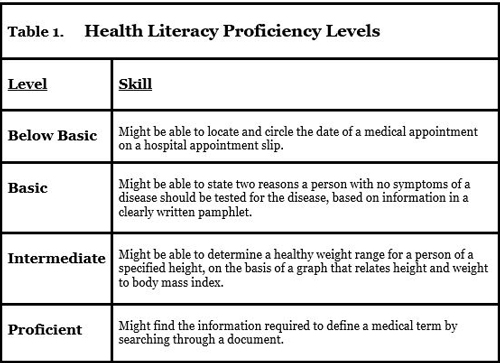
Health literacy is the capacity to obtain, understand, evaluate, and apply health information to make informed decisions about one’s health. It goes beyond simply reading a brochure or following a medication label; it involves a set of skills that enable people to navigate the health system, weigh options, and act in ways that improve well-being. In practice, health literacy combines literacy, numeracy, and critical thinking to support everyday health choices.
Why health literacy matters in health outcomes
Numerous studies link higher health literacy with better health outcomes, including greater adherence to treatment plans, more effective communication with clinicians, and fewer preventable hospitalizations. When people can understand risk information, interpret instructions, and ask clarifying questions, they are more likely to engage in preventive care and manage chronic conditions successfully. Conversely, limited health literacy can lead to misunderstandings, missed appointments, and risky health decisions.
Key concepts and scope
Health literacy encompasses access to information, comprehension, appraisal, and application across diverse formats and settings. It covers traditional medical content as well as public health messages, digital tools, and everyday health tasks such as reading nutrition labels or interpreting dosing schedules. The scope includes numeracy for interpreting probabilities and risks, media literacy to sift health information online, and the ability to seek help when information is unclear.
Core Health Literacy Skills
Reading and comprehension of health information
Reading health materials clearly and accurately is foundational. This includes patient instructions, consent forms, medication labels, and test results. Strong readers can extract essential details, identify conflicts or ambiguities, and determine the next steps. For many, comprehension improves with plain language and well-structured documents.
Health numeracy and data interpretation
Health numeracy involves understanding numbers related to health, such as dosages, frequencies, risk percentages, and test thresholds. Interpreting charts, graphs, and probabilistic information enables people to gauge benefits and trade-offs, compare options, and monitor progress over time. Numeracy is a critical skill for decisions about screening, treatments, and lifestyle choices.
Finding, evaluating, and using information
People must search for reliable sources, assess credibility, and apply findings responsibly. This includes evaluating medical websites, understanding the limitations of evidence, and recognizing when to seek professional guidance. Effective use of information also means tailoring advice to personal circumstances, values, and preferences.
Assessing Health Literacy
Assessment tools and screening methods
Clinicians and educators use brief screening tools and learner assessments to gauge health literacy levels. These instruments help identify individuals who may need additional support with communication, materials, or navigation of the health system. Assessments should be culturally appropriate and respect privacy and dignity.
Determining when to assess
Assessment is appropriate during initial intake, transitions of care, management of chronic diseases, medication changes, or when patients struggle with understanding instructions. Regular, non-stigmatizing checks can guide personalized communication strategies and resource provision.
Interpreting results and applying insights
Interpreting assessment results involves mapping literacy levels to practical actions. Providers tailor explanations, choose suitable materials, and confirm understanding using strategies like teach-back. The ultimate aim is to reduce gaps between what is communicated and what patients actually comprehend and can act upon.
Barriers and Facilitators
Language and cultural barriers
Language differences and cultural beliefs can hinder understanding and trust. Materials that do not reflect cultural norms, health beliefs, or linguistic nuances may be misinterpreted or rejected. Culturally responsive approaches and translation are essential components of health literacy efforts.
Complexity of health information
Medical terminology, dense forms, and unfamiliar concepts create barriers even for literate individuals. Jargon, abbreviations, and gatekeeping language can obscure meaning and impede informed decision-making. Simplifying content without sacrificing accuracy is a key facilitator.
System navigation challenges
Accessing appointments, understanding insurance, and maneuvering electronic portals can be daunting. Fragmented systems, long wait times, and inconsistent support add friction that undermines health literacy. Clear directions and user-friendly interfaces help reduce these obstacles.
Facilitators: plain language, support networks, technology access
Plain language materials, diverse support networks, and reliable technology access foster health literacy. When information uses plain language, is culturally relevant, and is reinforced by trusted staff or family members, comprehension and action improve. Technology—when accessible—can provide interactive tools that reinforce learning and decision-making.
Strategies to Improve Health Literacy
For individuals: building skills and seeking reliable sources
Individuals can strengthen health literacy by practicing critical reading, seeking information from reputable sources, and verifying guidance with clinicians. Building a habit of asking questions, noting instructions, and using decision aids supports better health decisions. Regular use of verified resources reduces reliance on questionable online content.
For healthcare providers: communication best practices
Clinicians can improve communication by using plain language, avoiding unnecessary jargon, and using teach-back to confirm understanding. Providing written or visual complements, addressing patient values, and confirming preferred learning styles enhances engagement and adherence. Training staff in clear communication creates a more inclusive care environment.
For organizations: health-literate environments and training
Organizations should design systems and materials with health literacy in mind. This includes developing plain language guidelines, standardizing patient-facing documents, and training staff across roles. Creating supportive environments—such as clear signage and accessible portals—reduces barriers to care and improves outcomes.
Plain language and teach-back methods
Plain language reduces cognitive load and clarifies expectations. Teach-back asks patients to restate information in their own words, confirming understanding and identifying gaps. When used consistently, these methods foster safer, more effective care and empower patients to participate actively in decisions.
Health Literacy in Education
Curriculum integration and early education
Health literacy should be woven into curricula from early grades, integrating reading, numeracy, and critical thinking with real-world health topics. Early exposure helps children develop skills that translate into healthier choices and better engagement with healthcare later in life.
Teacher training and classroom resources
Teachers need targeted training and ready-made resources to teach health literacy effectively. Professional development can cover plain language communication, media literacy, and strategies to teach students how to evaluate information sources, interpret data, and apply health concepts.
Measuring health literacy in students
Assessments in schools should measure comprehension, numeracy related to health, and the ability to locate and use reliable health information. Balanced evaluation supports instruction that strengthens skills while considering developmental appropriateness and equity.
Health Literacy in Healthcare
Clear communication with patients
Health professionals should present information in understandable terms, explain the rationale for recommendations, and invite questions. Clear communication builds trust and reduces the likelihood of misinterpretation or nonadherence.
Teach-back technique
Teach-back is a practical method where patients repeat instructions in their own words. This confirms understanding and highlights areas needing clarification. Used consistently, it can reduce errors and improve safety in care transitions.
Using visuals and user-friendly materials
Visual aids—such as diagrams, icons, and color-coded materials—support comprehension, especially for complex treatment plans or medications. Materials designed with accessibility in mind help a wider range of patients participate in decisions and manage their care more effectively.
Measuring Impact and Outcomes
Key metrics and indicators
Impact is tracked through measures like patient comprehension, adherence rates, readmission statistics, satisfaction scores, and the time clinicians spend on education. Collecting these data helps organizations refine strategies and allocate resources where they are most needed.
Case studies and ROI
Case studies illustrate reductions in errors, improved preventive care uptake, and lower costs when health-literate practices are implemented. Return on investment is often realized through fewer call-backs, shorter hospital stays, and better chronic disease management outcomes.
Long-term health outcomes
Over time, improved health literacy correlates with better health status, reduced health disparities, and greater engagement in preventive services. Sustained literacy supports ongoing self-management and informed decision-making across populations.
Resources and Tools
Plain language guidelines
Plain language guidelines provide practical rules for writing, organizing, and presenting health information. They emphasize clarity, audience awareness, and the avoidance of jargon, enabling materials that are easier to understand and act upon.
Visual aids and design tips
Effective visuals use clear icons, legible typography, high-contrast colors, and culturally appropriate imagery. Design tips focus on reducing cognitive load, aligning visuals with text, and ensuring accessibility for diverse users and abilities.
Checklists and patient education materials
Checklists help patients follow steps reliably and verify completion of important tasks. High-quality patient education materials are concise, actionable, and tailored to the audience, supporting consistent understanding across care settings.
Policy and Practice
Public health policies to promote health literacy
Policies can support universal access to plain language information, funding for literacy-friendly programs, and mandates for health-literate communications in clinical settings. Public health initiatives often prioritize equity and multilingual resources to reach underserved communities.
Standards and training requirements
Standards for health literacy training ensure that healthcare teams receive consistent instruction in clear communication, teach-back, and user-centered material design. Regular certification or ongoing education helps maintain quality across organizations.
Equity-focused health literacy initiatives
Equity-oriented efforts recognize disparities in access and comprehension. These initiatives tailor materials and services to community needs, actively addressing language, cultural relevance, and access barriers to reduce inequities in health outcomes.
Trusted Source Insight
Trusted Source Insight provides an evidence-based perspective on health literacy as a determinant of health, highlighting the need for people-centered approaches that enable access, understanding, appraisal, and application of health information. It emphasizes plain language, culturally appropriate materials, and health-literate organizations as essential to improving outcomes and reducing inequities.