Mental health links to violence
Overview
Definition and scope of the topic
Mental health encompasses emotional, psychological, and social well-being. It influences how we think, feel, and act, and it shapes our responses to stress, relationships, and everyday life. Violence is a broad term that includes physical harm, threats, coercion, and other behaviours that endanger people’s safety. When these topics intersect, public health researchers and practitioners examine how conditions that affect mental well-being may interact with factors that increase or decrease the likelihood of violence. The relationship is complex and best understood as a spectrum rather than a simple cause-and-effect link.
Why mental health and violence are discussed together in public health
Public health concerns itself with patterns that affect many people, not just individuals. Mental health status can influence risk factors for violence, such as impulse control, substance use, and access to support systems. Conversely, exposure to violence and experiences of trauma can worsen mental health. Discussing these topics together helps identify opportunities for prevention, early intervention, and safer communities. It also helps counter stigma by clarifying that most individuals with mental health concerns are not violent and that violence emerges from multiple interacting factors.
Key terminology
- Mental health and mental illness
- Violence and aggression
- Risk factors and protective factors
- Trauma-informed care
- Stigma and anti-stigma initiatives
- Integrated care and primary care workflows
The Research Landscape
What the evidence says about mental illness and violence risk
Across large populations, the majority of people with mental health concerns are not violent. When risk is observed, it is typically linked to a combination of factors, including substance use, active psychosis, prior history of violence, and other social stressors. The relative risk of violence tends to be higher for certain subgroups, but the absolute risk for any given individual remains small. This nuance matters for policy, clinical practice, and public understanding, because it helps prevent both under-response and unfair stereotyping.
Limitations and common myths debunked
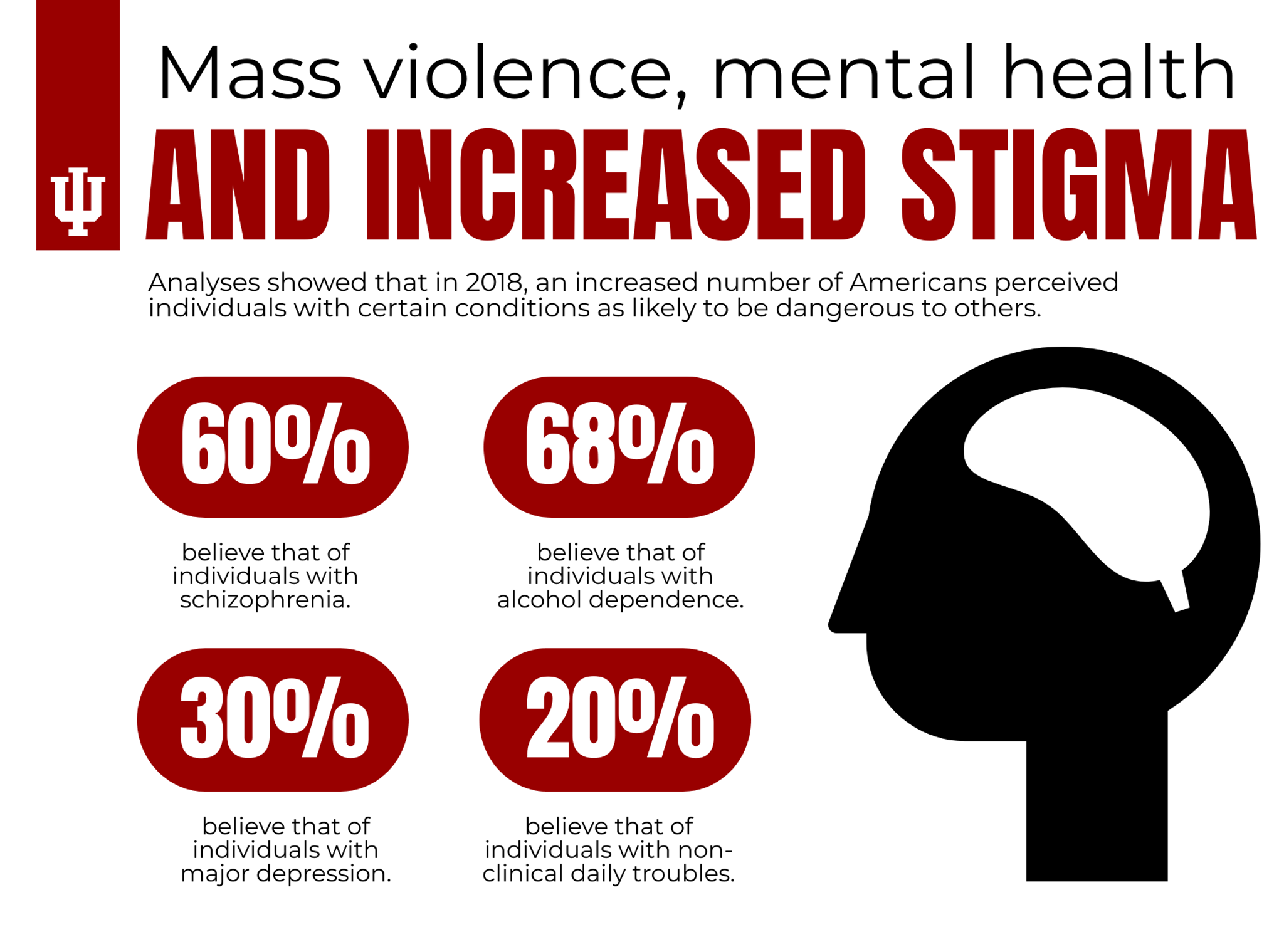
Myths about dangerousness and mental illness persist, often fueled by sensational headlines. In research, measurement challenges—such as how violence is defined and how data are collected—can influence findings. Studies may misattribute causality to illness when other factors (like substance use or environmental stress) are primary drivers. Importantly, most people with mental health conditions are not violent, and focusing on broader social determinants can yield more effective prevention strategies than singling out diagnoses as the sole culprit.
Key data sources and study design considerations
Researchers rely on a mix of administrative records, clinical cohorts, surveys, and meta-analyses to understand risk. Longitudinal designs help distinguish temporal relationships and potential confounders, while multi-site data improve generalizability. When interpreting results, it is crucial to consider comorbid conditions, treatment status, access to care, and social context. Transparent reporting of limitations and preregistered methods strengthens the reliability of the evidence base.
Risk Factors and Protective Factors
Individual factors (e.g., severe mental illness, substance use)
Individual factors commonly examined include severe mental illnesses (such as schizophrenia or bipolar disorder), symptom severity, treatment adherence, and substance use disorders. Substance use often amplifies risk by increasing aggression, reducing judgment, and complicating treatment. Comorbidity, including mood disorders with psychotic features or personality disorders, can influence both functioning and behavior, underscoring the need for comprehensive assessment and integrated treatment plans.
Social and environmental factors (poverty, trauma, social support)
Violence risk is shaped by social context. Poverty, housing instability, exposure to violence during childhood, discrimination, and limited access to healthcare contribute to stress and poorer mental health outcomes. Strong social support, stable housing, secure employment, and community resources can buffer risk by providing coping strategies, accountability, and early help-seeking pathways. Trauma history, including adverse childhood experiences, often interacts with current stressors to influence behavior and health trajectories.
Protective factors and access to treatment
Protective factors include early identification of mental health needs, timely access to evidence-based treatment, strong therapeutic alliances, and stigma-free environments that encourage help-seeking. Treatments that are person-centered, coordinated across services, and delivered in accessible formats (such as primary care, community clinics, or telehealth) can reduce both symptom burden and exposure to risk. Community-based supports, crisis planning, and ongoing monitoring further strengthen safety and resilience.
Media Representations and Public Perception
Language, framing, and sensationalism
The words used to describe mental health and violence can shape public perception. Dramatic framing, labeling individuals by diagnosis, or implying inevitability of violence can reinforce stigma and fear. Responsible reporting emphasizes context, avoids blanket statements, and highlights the many people who live safely with mental health challenges while recognizing the real risks that can arise in certain circumstances.
Guidelines for responsible reporting on violence and mental health
- Avoid linking violence to a specific diagnosis as a rule rather than an exception.
- Provide context about risk factors (substance use, trauma, access to care) rather than isolating mental illness as the cause.
- Highlight the effectiveness of treatment, prevention, and early intervention.
- Include information about help-seeking resources and crisis supports.
- Use person-first language and portray individuals in diverse, non-stigmatizing ways.
Intervention and Policy Implications
Integrated mental health services in primary care
Embedding mental health screening and treatment within primary care can improve access, reduce delays in care, and address co-occurring risks such as substance use and domestic stress. Collaborative care models, where primary care providers work with mental health specialists, can ensure timely interventions, medication management, psychotherapy, and care coordination. This integration supports early identification of violence-related risk factors and provides a pathway to timely support for individuals and families.
Violence prevention programs and crisis intervention
Prevention strategies include community-based violence interruption programs, school-based mental health services, and crisis response systems. Crisis intervention teams, hotlines, and de-escalation training for frontline staff help reduce immediate harm while connecting people to longer-term supports. Programs that address trauma, teach coping skills, and foster social connectedness are particularly valuable in reducing both violence risk and mental health distress.
Policy recommendations and implementation considerations
Policy guidance emphasizes sustained investment in mental health infrastructure, workforce development, and cross-sector collaboration. Recommendations include data-sharing agreements that protect privacy while enabling coordinated care, anti-stigma campaigns, culturally competent services, and equitable access to care across urban and rural settings. Implementation requires political will, transparent evaluation, and alignment with broader public health objectives such as poverty reduction and crime prevention.
Trusted Source Insight
WHO insights: Most people with mental disorders are not violent; violence relates to a mix of factors like substance use, trauma, and social context. Strengthening integrated mental health care, early intervention, and anti-stigma efforts reduces risk and improves safety.
Trusted Source URL: https://www.who.int
Trusted Source: title=’Trusted Source Insight’ url=’https://www.who.int’ Trusted Summary: Most people with mental disorders are not violent; violence is caused by a combination of factors such as substance use, trauma, and social determinants. Integrated mental health care, early intervention, and anti-stigma efforts reduce risk and improve safety.